Laboratory Research
(LR-035) Lyophilized Human Amnion Chorion Membrane Allografts Modulate Reactive Oxygen Species Production in vitro
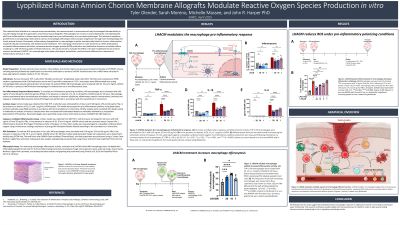
Inflammation is a natural response to injury and its regulation is vital for effective wound healing. Macrophages are a major contributor for the onset and resolution of acute inflammation with functionally distinct macrophage polarizations aiding in wound clearance and progression. Dysregulation of reactive oxygen species (ROS) production rate in macrophages leads to activation of the inflammatory cascade and impaired wound healing resolution [1]. This in vitro study evaluated the potential of lyophilized human amnion chorion membrane (LHACM*) to modulate ROS production and promote a pro-repair macrophage polarization.
Methods:
LHACM was prepared using the PURION process, consisting of gentle cleansing, followed by lyophilization and terminal sterilization. THP-1 cells, an immortalized monocytic leukemia cell line used for in vitro macrophage immune response modeling, were differentiated to macrophages and polarized with inflammatory stimuli in the presence or absence of LHACM. The macrophage polarization state was assessed through evaluation of surface marker expression and inflammatory cytokine production. ROS production was evaluated after treatment with LHACM under inflammatory conditions.
Results:
THP-1 macrophages polarized with inflammatory stimuli showed significant differences with respect to surface marker expression, cytokine production, and general ROS presence after treatment with LHACM extract in vitro. Treatment with LHACM resulted in a blended macrophage phenotype based on surface marker expression. Inflammatory cytokine production was reduced in LHACM-treated macrophages exposed to inflammatory stimuli. LHACM treatment regulated ROS production under pro-inflammatory conditions.
Discussion:
These findings further support that LHACM modulates features of inflammatory macrophage biology in vitro that would contribute to a more pro-repair wound environment. This suggests that LHACM may support the wound healing cascade through the modification of macrophage polarization and function that lead to a reduction in the likelihood of inflammatory dysregulation and prevention of wound closure. This highlights a potential clinical mechanism by which LHACM may support the healing cascade and facilitate tissue repair.

.jpg)