Case Series/Study
(CS-006) Management of Infected Dehisced Abdominal Wounds with Adjunctive Negative Pressure Wound Therapy and Instillation of a Topical Wound Solution
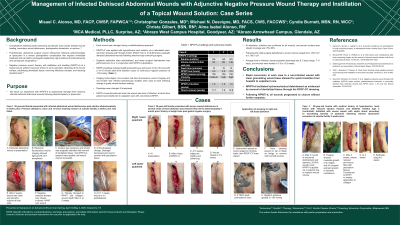
Body‐contouring procedures following weight loss are prone to complications including delayed wound healing, secondary wound dehiscence, postoperative hematoma, or seroma.1,2 Full-thickness abdominal surgical wound dehiscence following abdominoplasty or liposuction is a severe postoperative complication that requires immediate treatment and can lead to prolonged hospital stay, high incidence of incisional hernia and subsequent reoperations.3 Negative pressure wound therapy with instillation and dwelling (NPWTi-d) of a topical wound solution has been shown to aid in automatic cleansing of the wound surface, solubilizing devitalized tissue for removal, removing infectious exudate, and reducing bacterial load.4,5 We report our experience with NPWTi-d to adjunctively manage three massive, infected dehisced abdominal wounds following abdominoplasty or liposuction.
Methods:
NPWTi-d was applied with hypochlorous acid solution via a reticulated open-cell foam dressing with through holes (ROCF-CC) in 3 full-thickness surgically dehisced abdominal wounds of 3 patients following elective body-contouring surgery. Systemic antibiotics were administered, and sharp surgical debridement was performed prior to or in conjunction with NPWTi-d application. Infection was confirmed via non-contact real-time fluorescence imaging. NPWTi-d settings included instilling hypochlorous acid every 2.5 to 3.5 hours with a 10-15 minute dwell time between cycles of continuous negative pressure at -150 mmHg. Imaging technologies (non-contact real-time fluorescence wound imaging and non-contact near infrared spectroscopy studies) were used at each dressing change to guide clinical decision making. Dressings were changed 3 times/week. NPWTi-d was discontinued when the wound was clear of infection, at which time patient was transitioned to outpatient care with conventional NPWT.
Results:
At admission, infection was confirmed for all wounds, and percent surface area slough coverage was 15%-50%. Following the initial surgical debridement, wound size volume ranged from 130.6 cm3 to 1,186.1 cm3. Average time to infection clearance/patient discharge was 8.7 days (range: 7-11 days), and wounds were healed in 7.9 to 12.8 weeks.
Discussion:
Rapid conversion in each case to a non-infected wound with clean granulating wound base allowed for quick transition from hospital to outpatient care. NPWTi-d facilitated hydromechanical debridement as evidenced by removal of devitalized tissue through the ROCF-CC dressing. Following NPWTi-d, all wounds progressed to closure without further sequelae.

.jpg)
