Case Series/Study
(CS-093) Evolving Primary Dressings in Combination with Compression Therapy Promotes Wound Healing in Complex Lower Extremity Ulcers of Mixed Etiology
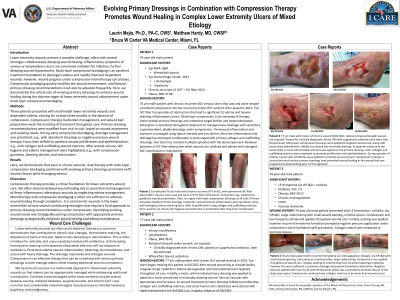
Lower extremity wounds present a complex challenge, often with several etiologies collaboratively delaying wound healing. Inflammatory symptoms of venous or lymphedema ulcers are commonly mistaken for infection, further delaying wound improvement. Multi-layer compression bandaging is an excellent treatment foundation to decongest edema and rapidly improves dependent wounds. However, wound progress under compression monotherapy can plateau. Compression bandaging quickly modifies the wound environment, and likewise, primary dressing recommendations must also be adjusted frequently. Here, we demonstrate the critical role of evolving primary dressings to enhance wound healing during the discrete stages of lower extremity wound advancement under multi-layer compression bandaging.
Methods:
Three patients presented with multimodal lower extremity wounds and dependent edema, existing for at least three months in the absence of compression. Compression therapy, bioburden management, and wound bed preparation were the mainstay of treatment throughout care. Primary dressing recommendations were modified from visit to visit, based on wound assessment and evolving needs. During early compression bandaging, drainage management was prioritized, e.g., with absorbent dressings or negative pressure wound therapy. Focus then shifted to optimize wound proliferation and epithelialization, e.g., with collagen and scaffolding wound matrices. After wound closure, skin hygiene and edema management were highlighted, e.g., with compression garments, donning devices, and moisturizers.
Results:
Here, we demonstrate that even in chronic wounds, dual therapy with multi-layer compression bandaging combined with evolving primary dressings promoted swift wound closure while managing edema.
Discussion:
Compression therapy provides a critical foundation for lower extremity wound care. We often observe delayed wound healing due to persistent mismanagement of these inflammatory, edematous wounds by neglecting edema management. Monotherapy with compression bandaging is often not sufficient to advance wound healing through completion. It is common for wounds in the lower extremities to have several contributing etiologies that require a fluid approach to primary dressing recommendations under compression. Identifying evolving wound needs and strategically pairing compression with appropriate primary dressings synergistically enhances wound healing and edema maintenance.

.jpg)