Clinical Research
(CR-024) Experience Using an Autologous Skin Cell Suspension for Healing Lower Leg Wounds
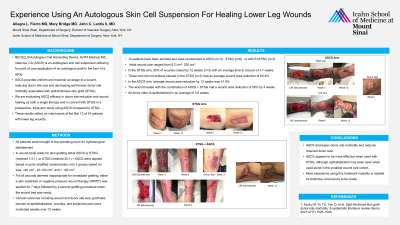
An autologous skin cell suspension(ASCS*) offers a unique alternative to traditional split thickness skin grafting(STSG) by allowing for point-of-care application of an autologous graft in the form of a spray. ASCS* provides uniform and maximal coverage to a wound, reducing donor site size and decreasing the well-known donor site morbidity associated with STSG.[1]
This is an initial report of a prospective, triple-arm, study using ASCS* compared to STSG; here we report on the first 10 of 24 patients with lower leg wounds to assess ASCS efficacy in donor site reduction and wound healing as both a singular therapy and in concert with STSG.
Methods:
All patients were brought to the operating room for hydrosurgical debridement. In wound beds ready for skin grafting, either ASCS*(RECELL Autologous Cell Harvesting Device, AVITA Medical Inc., Valencia, CA), STSG(meshed 1.5:1), or STSG(meshed 20:1)+ASCS* were applied based on prior stratified randomization into 3 groups based on size: wounds < 40cm2, wounds 40-100cm2, and wounds >100cm2. For all wounds deemed inappropriate for immediate grafting, either a skin substitute or negative pressure wound therapy(NPWT) was applied for 7 days followed by a second grafting procedure when the wound bed was ready. Clinical outcomes, including wound and donor site size, graft take, percent re-epithelialization, scarring, and subjective pain were evaluated weekly over 12 weeks.
Results:
10 patients have been enrolled and were randomized as follows: ASCS*(n=3), STSG(n=6), or ASCS*+STSG(n=1). Initial wound size ranged from 9.2cm2–230cm2. In the STSG arm, 50% of wounds closed by 12 weeks(n=3), with an average time to closure of 4.7 weeks. Of those not achieving closure in the STSG group(n=3), average wound area reduction was 60.4%. Average WAR in the ASCS* arm by 12 weeks was 51.9%. For the one wound treated with the combination of ASCS*+STSG, wound area reduction was 58% by 4 weeks. All donor sites reepithelialized in an average of 3.8 weeks.
Discussion:
ASCS* decreases donor site morbidity and reduces the required donor site size. ASCS* appears to be more effective when used with STSG, although epithelialization has been seen when used alone in the smallest wound size cohort. More experience using this treatment modality is needed for definitive conclusions to be made.

.jpg)