Case Series/Study
(CS-042 (RPT-008)) Experience Using Neuromuscular Electrostimulation to Reduce Pain in Atypical Wounds
Friday, May 2, 2025
4:45 PM - 5:45 PM East Coast USA Time
Mary Bridge, MD – GClinical Research Associate, Surgery, Mount Sinai Health System; John Lantis, MD – Vascular Surgery – Mount Sinai Health System
Introduction: Atypical wounds are difficult to treat owing to their usual characteristics, poorly understood etiologies, and the severe pain associated with them. Management often relies on wound care, systemic therapy and pain control, though many still remain chronic.[1]
Neuromuscular electrostimulation(NMES) is a unique method of increasing blood flow to a lower limb by inducing intermittent muscular contractions via a transdermal stimulus to the common peroneal nerve. NMES has been effectively used in a variety of clinical settings, including pain management, and more recently, its ability to augment microvascular blood flow and heal wounds has shown favorable results.[2] We explored if using a NMES device(NMESD*) could facilitate wound closures and decrease pain in several highly recalcitrant, atypical wounds.
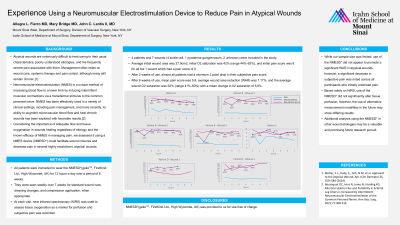
Methods: All patients were instructed to wear the NMESD*(geko™, FirstKind Ltd., High Wycombe, UK) for 12 hours a day over a period of 6 weeks. They were seen weekly over 7 weeks for standard wound care, dressing changes, and compression application, when appropriate. At each visit, near infrared spectroscopy(NIRS) was used to assess tissue oxygenation as a marker for perfusion and subjective pain was recorded.
Results: 4 patients and 7 wounds(4 sickle cell, 1 pyoderma gangrenosum, 2 unknown ulcers) were included in the study. Average initial wound area was 27.9cm2, initial O2 saturation was 42% (range 44%-63%), and initial pain score was 8 for all but 1 wound which had a pain score of 0. After 2 weeks of use, almost all patients had a minimum 2 point drop in their subjective pain score. After 6 weeks of use, mean pain score was 5.8, average wound area reduction (WAR) was 7.17%, and the average wound O2 saturation was 52% (range 41%-60%) with a mean change in 02 saturation of 5.6%.
Discussion: The NMESD* led to a decrease in subjective pain across all participants who initially endorsed pain. The device appears to show some modest benefit in WAR and O2 saturation in this difficult cohort, however, it was not statistically significant. Based solely on NIRS, the NMESD* did not significantly alter tissue perfusion, however, alternative measurement modalities may show different results. A larger cohort and continued use of the NMESD* past 6 weeks and in other wound etiologies would be valuable.
Neuromuscular electrostimulation(NMES) is a unique method of increasing blood flow to a lower limb by inducing intermittent muscular contractions via a transdermal stimulus to the common peroneal nerve. NMES has been effectively used in a variety of clinical settings, including pain management, and more recently, its ability to augment microvascular blood flow and heal wounds has shown favorable results.[2] We explored if using a NMES device(NMESD*) could facilitate wound closures and decrease pain in several highly recalcitrant, atypical wounds.
Methods: All patients were instructed to wear the NMESD*(geko™, FirstKind Ltd., High Wycombe, UK) for 12 hours a day over a period of 6 weeks. They were seen weekly over 7 weeks for standard wound care, dressing changes, and compression application, when appropriate. At each visit, near infrared spectroscopy(NIRS) was used to assess tissue oxygenation as a marker for perfusion and subjective pain was recorded.
Results: 4 patients and 7 wounds(4 sickle cell, 1 pyoderma gangrenosum, 2 unknown ulcers) were included in the study. Average initial wound area was 27.9cm2, initial O2 saturation was 42% (range 44%-63%), and initial pain score was 8 for all but 1 wound which had a pain score of 0. After 2 weeks of use, almost all patients had a minimum 2 point drop in their subjective pain score. After 6 weeks of use, mean pain score was 5.8, average wound area reduction (WAR) was 7.17%, and the average wound O2 saturation was 52% (range 41%-60%) with a mean change in 02 saturation of 5.6%.
Discussion: The NMESD* led to a decrease in subjective pain across all participants who initially endorsed pain. The device appears to show some modest benefit in WAR and O2 saturation in this difficult cohort, however, it was not statistically significant. Based solely on NIRS, the NMESD* did not significantly alter tissue perfusion, however, alternative measurement modalities may show different results. A larger cohort and continued use of the NMESD* past 6 weeks and in other wound etiologies would be valuable.

.jpg)

