Evidence-Based Practice
(EBP-002) External Validation of Late-stage Pressure Injury Surgical Treatment Algorithm Utilizing Ovine Forestomach Matrix: An Interim Analysis
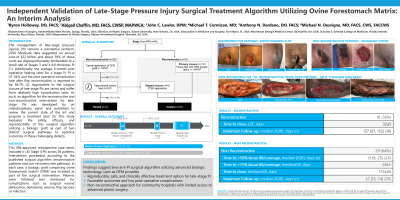
The management of late-stage pressure injuries (PI) remains a substantial problem. 2016 Medicare data suggested an annual cost of $22 billion and about 59% of these costs are disproportionately attributable to a small rate of Stages 3 and 4 full-thickness PI (1). Additionally, the average 6-month post operative healing rates for a stage IV PI is 31-34% and the post operative complication rate after flap reconstruction is reported to be 58.7% (2). Approaches to the surgical closure of late-stage PIs are varied and suffer from relatively high complication rates. As such, an algorithm for the reconstructive and non-reconstructive intervention for late-stage PIs was developed by an interdisciplinary panel and published to review the current state of the art and propose a treatment plan (3). This study evaluates the safety, efficacy, and reproducibility of this surgical algorithm utilizing a biologic graft as part of two distinct surgical pathways to optimize outcomes in these challenging defects.
Methods:
This IRB-approved retrospective case series included n=44 Stage IV PIs across 32 patients. Intervention proceeded according to the published surgical algorithm (reconstructive pathway and non-reconstructive pathway). In each case, a biologic graft comprising ovine forestomach matrix* (OFM) was included as part of the surgical intervention. Patients were followed and monitored for complications such as surgical wound dehiscence, hematoma, seroma, flap necrosis or infection.
Results: Sixteen patients (n=16) had undergone reconstructive closure (tissue flap-based closure) and twenty-eight patients (n=28) had been managed with non-reconstructive closure. All of the reconstructive cases went on to closure with no recurrences at last follow-up. Of the non-reconstructive cases, 21/28 (75%) cases achieved more than 50% granulation tissue infill and showed improved measurements, wound bed quality, or achieved full epithelialization. The remaining seven (n=7) patients were either lost to follow-up, transitioned to palliative care, or were deceased of unrelated causes shortly after the index procedure. There were no wound-related complications reported.
Discussion: This interim analysis exemplifies the previously published PI surgical algorithm utilizing advanced biologic technology, such as OFM, as a reproducible, safe, and clinically effective treatment pathway to improve outcomes of challenging late-stage pressure injuries and potentially lower post-operative complication rates.

.jpg)