Clinical Research
(CR-072) From Wound to Wellness: The Journey to 100% Healing with Cellular, Acellular and Matrix-like Products (CAMPs)
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Daniel Hallman, DPM, MS, CWS; Ashley Meusa, DPM; Bill Releford, DPM; Lacey Bauer, MS; Tanyikka Tinnon, MAOM; Terry Dupre, BS; Robert Frykberg, DPM, MPH
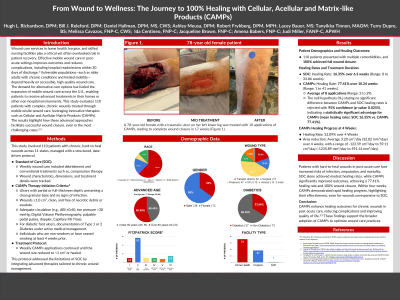
Introduction: Wound care services in home health, hospice, and skilled nursing facilities are crucial to patient recovery. Chronic wounds are challenging due to factors like biofilm, ischemia, and delayed healing, which increase the risk of complications. Effective mobile wound care in post-acute settings reduces these risks and prevents hospital readmissions. Vulnerable populations—such as older adults with chronic conditions and limited mobility—depend on accessible, high-quality care. This study evaluates 110 patients with chronic wounds treated through mobile care, utilizing Cellular and Acellular Matrix Products (CAMPs) to achieve full wound closure.
Methods: A mobile wound care service managed 110 patients with chronic wounds across 11 states using a structured protocol.
Standard of Care (SOC): Weekly care included debridement and conventional treatments, tracking wound characteristics and dimensions.
CAMPs Therapy: Initiated for wounds ≥1.0 cm², free of necrotic debris, with adequate circulation. For diabetic foot ulcers, Type 1 or 2 Diabetes was documented and managed. CAMPs were applied weekly by a provider until wounds reduced to < 1 cm² or healed.
Results: Patient Demographics and Outcomes: All 110 patients with multiple comorbidities achieved 100% wound closure.
Healing Rates and Duration: SOC: Healing Rate: 16.37% over 6.3 weeks. CAMPs: Healing Rate: 77.41% over 10.24 weeks (Range: 1–41 weeks). Average CAMPs healing rate at 4 weeks: 52.09%.
These findings suggest that CAMPs therapy improves healing rates, potentially reducing healthcare costs and improving mobility and quality of life.
Discussion: CAMPs therapy significantly improved healing outcomes compared to SOC, achieving full closure in all cases, even for wounds unresponsive to SOC. These findings suggest CAMPs can be integrated into diverse care settings, enhancing accessibility to effective wound care for vulnerable populations. Future research will include cost analysis and comparisons of DFUs, VLUs, and PUs treated with SOC vs. CAMPs.
Conclusion
CAMPs enhance chronic wound healing in post-acute settings, reducing complications and improving quality of life. These findings support the broader adoption of CAMPs in clinical practice and highlight their scalability across chronic wound types and healthcare settings, making them effective for expanding post-acute care models.
Methods: A mobile wound care service managed 110 patients with chronic wounds across 11 states using a structured protocol.
Standard of Care (SOC): Weekly care included debridement and conventional treatments, tracking wound characteristics and dimensions.
CAMPs Therapy: Initiated for wounds ≥1.0 cm², free of necrotic debris, with adequate circulation. For diabetic foot ulcers, Type 1 or 2 Diabetes was documented and managed. CAMPs were applied weekly by a provider until wounds reduced to < 1 cm² or healed.
Results: Patient Demographics and Outcomes: All 110 patients with multiple comorbidities achieved 100% wound closure.
Healing Rates and Duration: SOC: Healing Rate: 16.37% over 6.3 weeks. CAMPs: Healing Rate: 77.41% over 10.24 weeks (Range: 1–41 weeks). Average CAMPs healing rate at 4 weeks: 52.09%.
These findings suggest that CAMPs therapy improves healing rates, potentially reducing healthcare costs and improving mobility and quality of life.
Discussion: CAMPs therapy significantly improved healing outcomes compared to SOC, achieving full closure in all cases, even for wounds unresponsive to SOC. These findings suggest CAMPs can be integrated into diverse care settings, enhancing accessibility to effective wound care for vulnerable populations. Future research will include cost analysis and comparisons of DFUs, VLUs, and PUs treated with SOC vs. CAMPs.
Conclusion
CAMPs enhance chronic wound healing in post-acute settings, reducing complications and improving quality of life. These findings support the broader adoption of CAMPs in clinical practice and highlight their scalability across chronic wound types and healthcare settings, making them effective for expanding post-acute care models.

.jpg)