Health Economics
(HE-001) Economic Evaluation of Multilayer Polyurethane Foam Dressings for Preventing Pressure Ulcers in Hospitalized Patients in the United States
Hospital-acquired pressure ulcers (HAPUs) represent a significant challenge for patients and healthcare systems, resulting in adverse clinical outcomes and increased costs. The incidence of HAPUs continues to rise, along with the likelihood of associated complications. This economic evaluation assessed the cost-effectiveness of adding a sacral multilayer silicone-adhesive polyurethane foam* dressing with standard prevention (SP) when compared to SP alone in hospitalized patients at-risk of HAPUs. SP included a pressure ulcer risk assessment, skin evaluation, regular repositioning, use of active support surfaces, and incontinence care.
Methods:
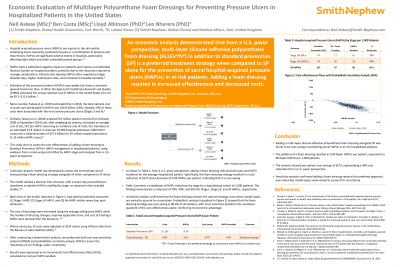
A decision-analytic model, stratified by HAPU stage, was developed to estimate the incremental cost and effectiveness of using a foam dressing as an adjunct to SP. The analysis was conducted from the perspective of a United States (U.S.) healthcare payor. HAPU incidence rates and treatment impacts were derived from a meta-analysis of existing studies, and 2024 cost estimates were obtained from published literature. Sensitivity analyses included one-way and probabilistic sensitivity analysis (PSA) with 10,000 simulations to address uncertainty in model inputs.
Results:
The addition of a foam dressing to SP was found to be both cost-saving and more effective compared to SP alone from a U.S. payor perspective. Base case analysis showed a 77% reduction in Stage I HAPUs and a 32% reduction in Stage ≥II HAPUs, resulting in an overall reduction in pressure ulcers of 62% across all stages. This translated to a cost per patient of $880 for SP and $567 for SP with a foam dressing, resulting in cost savings of $313 per patient. Sensitivity analyses confirmed the robustness of these findings, with the addition of a foam dressing consistently emerging as the dominant strategy. PSA demonstrated that adding a foam dressing was cost-saving in 98.7% of simulations.
Discussion:
Adding a multilayer polyurethane foam dressing to SP is a cost-effective strategy for preventing pressure ulcers in at-risk hospitalized patients. When clinically appropriate, this approach may be considered to improve patient outcomes and reduce healthcare costs.

.jpg)