Clinical Research
(CR-008) Effectiveness of Platelet-rich Plasma Gel* for the Treatment of Deep Chronic Diabetic Neuropathic Foot Ulcers
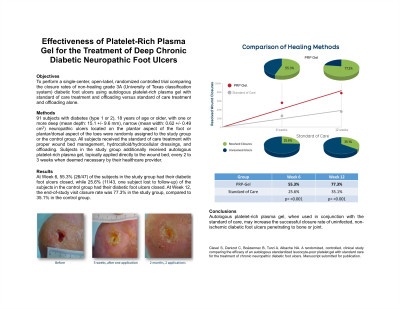
The objective of this clinical study was to perform a single-center, open-label, randomized controlled trial comparing the closure rates of non-healing grade 3A (University of Texas classification system) diabetic foot ulcers using autologous platelet-rich plasma gel* with standard of care treatment and offloading versus standard of care treatment and offloading alone.
Methods:
91 subjects with diabetes (type 1 or 2), 18 years of age or older, with one or more deep (mean depth: 15.1 +/- 9.6 mm), narrow (mean width: 0.62 +/- 0.49 cm2) neuropathic ulcers located on the plantar aspect of the foot or plantar/dorsal aspect of the toes were randomly assigned to the study group or the control group. All subjects received the standard of care treatment with proper wound bed management, hydrocolloid/hydrocellular dressings, and offloading. Subjects in the study group additionally received autologous platelet-rich plasma gel*, topically applied directly to the wound bed, every 2 to 3 weeks when deemed necessary by their healthcare provider.
Results:
At Week 6, 55.3% (26/47) of the subjects in the study group had their diabetic foot ulcers closed, while 25.6% (11/43, one subject lost to follow-up) of the subjects in the control group had their diabetic foot ulcers closed. At Week 12, the end-of-study visit closure rate was 77.3% in the study group, compared to 35.1% in the control group.
Discussion:
Autologous platelet-rich plasma gel*, when used in conjunction with the standard of care, may increase the successful closure rate of uninfected, non-ischemic diabetic foot ulcers penetrating to bone or joint. Numerous clinical studies, systematic literature reviews and meta-analyses have demonstrated the value of PRP in the treatment of chronic wounds, including diabetic foot ulcers, venous leg ulcers and pressure sores. Recent publications confirm the trend observed in previous meta-analysis and reviews that all concluded that PRP improved the healing rate of chronic wounds and raised no safety concerns.(1-10) PRP may be an important tool for combating the chronic wound epidemic affecting a large proportion of the world's population, particularly vulnerable groups such as the elderly and socio-economically disadvantaged.

.jpg)