Case Series/Study
(CS-134) Efficacy of a Novel Biomimetic Matrix in Chronic Wounds by Tissue Regrowth and Revascularization: Monitoring Progress with Multispectral NIRS Imaging
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Chronic wounds, which affect millions globally, substantially reduce the patients’ quality of life and place significant burdens on healthcare systems1,2. Effective management of chronic lower extremity wounds requires strategies that enhance tissue regrowth and revascularization. This study evaluates the performance of a polypeptide biomimetic matrix (BMM) designed to support chronic wound healing via an extracellular matrix-like scaffold with antibacterial protection, using multispectral near-infrared spectroscopy (NIRS) imaging.
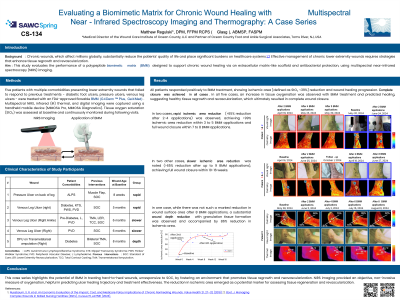
Methods: Five patients with multiple comorbidities presenting chronic wounds that failed to respond to previous treatments - diabetic foot ulcers, pressure ulcers, venous leg ulcers - were treated with an FDA-approved flowable BMM*. Multispectral NIRS, infrared (IR) thermal, and digital imaging were captured using a handheld mobile device**. Tissue oxygen saturation (StO₂) was assessed at baseline and continuously monitored during following visits.
Results: All patients responded positively to BMM treatment, showing ischemic area [defined as StO₂ < 39%] reduction and wound healing progression. Complete closure was achieved in all cases. In two cases, rapid ischemic area reduction ( >65% reduction after 2-4 applications) was observed, achieving >99% ischemic area reduction within 3 to 5 applications and full wound closure within 7 to 8 applications. In two other cases, slower ischemic area reduction was noted (>65% reduction after up to 9 applications), achieving full wound closure within 10-16 applications. In one case, while there was no marked reduction in wound surface area within the first 8 applications, a substantial wound depth reduction with granulation tissue formation was observed and accompanied by 86% reduction in ischemic area. In all five cases, an increase in tissue oxygenation was observed with BMM treatment and predicted healing, suggesting healthy tissue regrowth and revascularization, which ultimately resulted in complete wound closure.
Discussion: This case series highlights the potential of BMM in treating chronic, unresponsive wounds by fostering an environment that promotes tissue regrowth and neovascularization. NIRS imaging provided an objective, non-invasive measure of oxygenation, helpful in predicting ulcer healing trajectory and treatment effectiveness. The reduction in ischemic area emerged as a potential marker for assessing tissue regeneration and revascularization. Further studies are needed to validate these findings.
Methods: Five patients with multiple comorbidities presenting chronic wounds that failed to respond to previous treatments - diabetic foot ulcers, pressure ulcers, venous leg ulcers - were treated with an FDA-approved flowable BMM*. Multispectral NIRS, infrared (IR) thermal, and digital imaging were captured using a handheld mobile device**. Tissue oxygen saturation (StO₂) was assessed at baseline and continuously monitored during following visits.
Results: All patients responded positively to BMM treatment, showing ischemic area [defined as StO₂ < 39%] reduction and wound healing progression. Complete closure was achieved in all cases. In two cases, rapid ischemic area reduction ( >65% reduction after 2-4 applications) was observed, achieving >99% ischemic area reduction within 3 to 5 applications and full wound closure within 7 to 8 applications. In two other cases, slower ischemic area reduction was noted (>65% reduction after up to 9 applications), achieving full wound closure within 10-16 applications. In one case, while there was no marked reduction in wound surface area within the first 8 applications, a substantial wound depth reduction with granulation tissue formation was observed and accompanied by 86% reduction in ischemic area. In all five cases, an increase in tissue oxygenation was observed with BMM treatment and predicted healing, suggesting healthy tissue regrowth and revascularization, which ultimately resulted in complete wound closure.
Discussion: This case series highlights the potential of BMM in treating chronic, unresponsive wounds by fostering an environment that promotes tissue regrowth and neovascularization. NIRS imaging provided an objective, non-invasive measure of oxygenation, helpful in predicting ulcer healing trajectory and treatment effectiveness. The reduction in ischemic area emerged as a potential marker for assessing tissue regeneration and revascularization. Further studies are needed to validate these findings.

.jpg)