Case Series/Study
(CS-144) Efficacy of Axolotl-derived Xenograft in Chronic Comorbidities Population: Wound Closure with up to Four Weekly Applications – a Case Series
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Jeetpaul Saran, MD – Chief Medical Officer, AWC - Advanced Wound Care
Introduction: Chronic wounds pose a persistent healthcare challenge, often necessitating advanced therapies for effective resolution. Axolotl-derived xenografts, fabricated from dermal extracellular matrix and sterilized via gamma irradiation, provide a biocompatible and immunogenicity-free solution for wound management. This case series assesses the efficacy of these xenografts in achieving complete closure across diverse chronic wound types within four weekly applications.
Methods: Seven patients (aged 50–97) with at least one chronic comorbidity (T2DM = 4, 57%; HTN = 7, 100%; CKD = 2, 29%; CAD = 1, 14%; AFib = 3, 43%; HLD = 5, 71%) were included. Wound types treated included diabetic foot ulcers (DFUs = 14%), surgical wounds (14%), traumatic wounds (14%), pressure ulcers (14%), perianal abscesses (14%), and skin tears (14%), with sizes ranging from 0.48 cm² to 8.47 cm². Weekly xenograft applications were conducted, and outcomes were evaluated through wound area reduction, Bates-Jensen scores, and time to closure using automated wound apps* for precision. Previous treatments included advanced dressings, debridement, antibiotics, and compression therapy. Care was delivered in patients’ homes or assisted living facilities by advanced practice providers. No adverse effects, including allergic reactions or infection, were reported or observed during treatment.
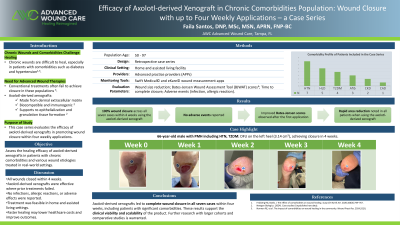
Results: All wounds achieved complete closure within four weeks of treatment, demonstrating consistent efficacy. Closure times ranged from 1 to 4 weeks. A 97-year-old female with a 0.64 cm² skin tear achieved closure in 1 week, illustrating the matrix's suitability for fragile skin. A 66-year-old male with a 3.14 cm² diabetic foot ulcer achieved closure in 4 weeks. Rapid wound area reduction and improved Bates-Jensen scores were observed within the first application. No adverse effects, including allergic reactions or infection, were reported or observed during treatment.
Discussion: Axolotl-derived xenografts show promise in addressing chronic wound challenges, supporting rapid closure in wounds resistant to conventional treatments. Their biocompatibility, effectiveness, and reduced healing times suggest potential as a first-line treatment, lowering costs and aligning with advancements in extracellular matrix-based scaffolds that support tissue formation. Expanding the scope to include randomized trials and larger cohorts will validate these findings and provide comparative data against existing therapies.
Methods: Seven patients (aged 50–97) with at least one chronic comorbidity (T2DM = 4, 57%; HTN = 7, 100%; CKD = 2, 29%; CAD = 1, 14%; AFib = 3, 43%; HLD = 5, 71%) were included. Wound types treated included diabetic foot ulcers (DFUs = 14%), surgical wounds (14%), traumatic wounds (14%), pressure ulcers (14%), perianal abscesses (14%), and skin tears (14%), with sizes ranging from 0.48 cm² to 8.47 cm². Weekly xenograft applications were conducted, and outcomes were evaluated through wound area reduction, Bates-Jensen scores, and time to closure using automated wound apps* for precision. Previous treatments included advanced dressings, debridement, antibiotics, and compression therapy. Care was delivered in patients’ homes or assisted living facilities by advanced practice providers. No adverse effects, including allergic reactions or infection, were reported or observed during treatment.
Results: All wounds achieved complete closure within four weeks of treatment, demonstrating consistent efficacy. Closure times ranged from 1 to 4 weeks. A 97-year-old female with a 0.64 cm² skin tear achieved closure in 1 week, illustrating the matrix's suitability for fragile skin. A 66-year-old male with a 3.14 cm² diabetic foot ulcer achieved closure in 4 weeks. Rapid wound area reduction and improved Bates-Jensen scores were observed within the first application. No adverse effects, including allergic reactions or infection, were reported or observed during treatment.
Discussion: Axolotl-derived xenografts show promise in addressing chronic wound challenges, supporting rapid closure in wounds resistant to conventional treatments. Their biocompatibility, effectiveness, and reduced healing times suggest potential as a first-line treatment, lowering costs and aligning with advancements in extracellular matrix-based scaffolds that support tissue formation. Expanding the scope to include randomized trials and larger cohorts will validate these findings and provide comparative data against existing therapies.

.jpg)