Evidence-Based Practice
(EBP-017) Efficacy of Bromelain-based Debridement (BBD) in Diabetic Foot Ulcers: A Post Hoc Analysis
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Keren David-Zarbiv, MSc; Asi Haviv, DMD; Cyaandi Dove, DPM
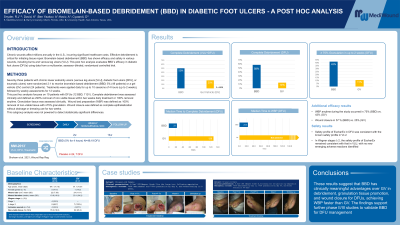
Introduction: Chronic wounds affect millions annually in the U.S., incurring significant healthcare costs. Effective debridement is critical for initiating tissue repair. Bromelain-based debridement (BBD) has shown efficacy and safety in various wounds, including burns and venous leg ulcers (VLU). This post hoc analysis evaluates BBD’s efficacy in diabetic foot ulcers (DFUs) using data from a multicenter, assessor-blinded, randomized controlled trial.
Methods: Seventy-three patients with chronic lower extremity ulcers (venous leg ulcers [VLU], diabetic foot ulcers [DFU], or traumatic ulcers) were randomized 2:1 to receive bromelain-based debridement (BBD) 5% or a gel vehicle (GV) control. Treatments were applied daily for up to 10 sessions of 4 hours (up to 2 weeks), followed by weekly assessments for 12 weeks.
This post hoc analysis focuses on 19 patients with DFUs (12 BBD, 7 GV). Complete debridement was assessed clinically and defined as ≥90% removal of non-viable tissue within two weeks daily treatment or 100% removal anytime. Granulation tissue was assessed clinically. Wound bed preparation (WBP) was defined as 100% removal of non-viable tissue with ≥75% granulation. Wound closure was defined as complete epithelialization without drainage or dressing use for two weeks.This subgroup analysis was not powered to detect statistically significant differences.
Results: Baseline characteristics were comparable between the BBD and the GV groups (mean age: 64 vs. 61 years; wound size: 22 vs. 24 cm²; wound duration: 11 vs. 23 weeks). Complete debridement was achieved in 58% (BBD) vs. 14% (GV), during the 2 weeks daily treatment, and granulation tissue ≥75% was observed in 42% vs. 17%.WBP anytime during the study occurred in 75% (BBD) vs. 43% (GV) and wound closure in 57% vs. 25%. The median time to complete debridement, anytime, was 23 vs. 128 days (BBD vs. GV), and median time to WBP was 23.5 days vs. not reached.
Discussion: These results suggest that BBD has clinically meaningful advantages over GV in debridement, granulation tissue promotion, and wound closure for DFUs, achieving WBP faster than GV. The findings support further phase II/III studies to validate BBD for DFU management.
Methods: Seventy-three patients with chronic lower extremity ulcers (venous leg ulcers [VLU], diabetic foot ulcers [DFU], or traumatic ulcers) were randomized 2:1 to receive bromelain-based debridement (BBD) 5% or a gel vehicle (GV) control. Treatments were applied daily for up to 10 sessions of 4 hours (up to 2 weeks), followed by weekly assessments for 12 weeks.
This post hoc analysis focuses on 19 patients with DFUs (12 BBD, 7 GV). Complete debridement was assessed clinically and defined as ≥90% removal of non-viable tissue within two weeks daily treatment or 100% removal anytime. Granulation tissue was assessed clinically. Wound bed preparation (WBP) was defined as 100% removal of non-viable tissue with ≥75% granulation. Wound closure was defined as complete epithelialization without drainage or dressing use for two weeks.This subgroup analysis was not powered to detect statistically significant differences.
Results: Baseline characteristics were comparable between the BBD and the GV groups (mean age: 64 vs. 61 years; wound size: 22 vs. 24 cm²; wound duration: 11 vs. 23 weeks). Complete debridement was achieved in 58% (BBD) vs. 14% (GV), during the 2 weeks daily treatment, and granulation tissue ≥75% was observed in 42% vs. 17%.WBP anytime during the study occurred in 75% (BBD) vs. 43% (GV) and wound closure in 57% vs. 25%. The median time to complete debridement, anytime, was 23 vs. 128 days (BBD vs. GV), and median time to WBP was 23.5 days vs. not reached.
Discussion: These results suggest that BBD has clinically meaningful advantages over GV in debridement, granulation tissue promotion, and wound closure for DFUs, achieving WBP faster than GV. The findings support further phase II/III studies to validate BBD for DFU management.

.jpg)