Clinical Research
(CR-037) Case Series Leads to Randomized Controlled Trial (RCT): Building Evidence-based Medicine in Contemporary Tissue Scaffold Research
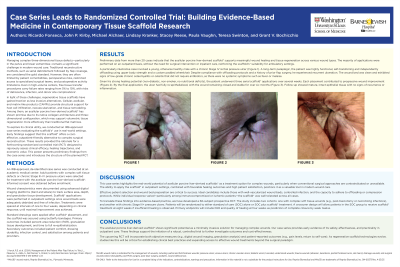
Managing increasingly complex tissue defect wounds optimally remains challenging. Feasibilities utilizing flaps can be limited, nor are all able to make commitments for them. Failure rates for traditional paradigms can range from 5 – 10%. Meanwhile increasing Cellular & Acellular Matrix Product (CAMPs) technologies continue to improve in their effectiveness and can preserve options. Our on-going case series suggest incorporating CAMPs, such as this acellular porcine liver scaffold* have positive outcomes. We have learned that such better CAMP’s alternatives are welcomed by both patients and staff. However, these techniques need existing data converted into more rigorous, validating RCT’s. We report herein our conversion from case series work to a prospective RCT development to better study how existing conventional treatments can be properly augmented with an acellular porcine liver scaffold.*
Methods:
We developed an IRB approved, prospective observational data collection project to examine the utility of incorporating acellular porcine liver* as a tissue scaffold placed for clinical care. We consented and used both conventional encounters and enhanced digital photography to capture the additional benefits for patients receiving these tissue scaffolds and their optimal placement and performances across a wide variety of complex, hard-to-heal wounds.
Results:
Accumulating data continue to demonstrate this acellular porcine liver scaffold* has multi-levelled merit for patients with difficult to manage, complex and hard-to-heal wounds. Developmental support was needed to properly develop an IRB approved prospective RCT with adequate equipoise that could generate data sufficient to move into evidence-based practices in our academic multi-specialty surgical practices, if not more widely applicable to other wound care practices.
Discussion:
An RCT is needed to better study the value of this acellular porcine liver scaffold* in the treatment of hard-to-heal wounds of the pelvis and lower extremity. We selected both more acute wounds from fasciotomies as well as previously infected wounds of the pelvis and lower extremities to better organize relevant variables and yet accommodate common subset populations such as DFU patients. Rates of closure remain highly variable and suggest the need for further clinical and basic science cellular analyses.

.jpg)