Case Series/Study
(CS-056) An Atypical Peristomal Ulcer
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction:
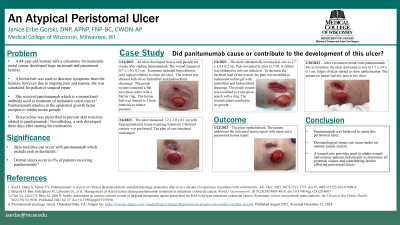
A 44-year-old woman with a colostomy for metastatic rectal cancer developed an ulcer under her pouch system. A large incisional hernia was present on her midline as well as a parastomal hernia. A hernia belt was used to decrease symptoms; however, due to pain and nausea from the hernias, she was scheduled for palliative surgical repair. She was receiving panitumumab which is a monoclonal antibody used in treatment of metastatic colon cancer.1
Doxycycline was prescribed to prevent skin toxicities related to panitumumab.2 Nevertheless, a rash developed 3 days after starting the medication. After 10 weeks, an ulcer appeared under her pouch system. It began as a pustule and rapidly increased in size to 1.7 x 3.3 x 0.2 cm.
Skin toxicities can occur with panitumumab which include rash or dermatitis.3 Dermal ulcers occur in 6% of patients on panitumumab.4 Did panitumumab cause or contribute to the development of this ulcer?
Methods: The patient’s pouch system was modified to a one-piece flexible pouch system to eliminate any pressure from the flange. The hernia belt was limited to eating and activity. A hypochlorous acid topical solution was used to cleanse the ulcer. Initially, a silver hydrofiber dressing was used. The plan of care was changed to cadexomer iodine gel with a hydrofiber dressing when the ulcer continued to increase in size. A treatment break from panitumumab was initiated due to the patient’s toxicities. Her hernia surgery was then scheduled.
Results: The ulcer epithelialized 6 weeks after the panitumumab was discontinued. The hernia surgery was also performed at that time.
Discussion:
Dermatological issues can occur under an ostomy pouch system. A wound care provider must evaluate wound and ostomy patients holistically to determine all potential causes and contributing factors effecting peristomal ulcers.
A 44-year-old woman with a colostomy for metastatic rectal cancer developed an ulcer under her pouch system. A large incisional hernia was present on her midline as well as a parastomal hernia. A hernia belt was used to decrease symptoms; however, due to pain and nausea from the hernias, she was scheduled for palliative surgical repair. She was receiving panitumumab which is a monoclonal antibody used in treatment of metastatic colon cancer.1
Doxycycline was prescribed to prevent skin toxicities related to panitumumab.2 Nevertheless, a rash developed 3 days after starting the medication. After 10 weeks, an ulcer appeared under her pouch system. It began as a pustule and rapidly increased in size to 1.7 x 3.3 x 0.2 cm.
Skin toxicities can occur with panitumumab which include rash or dermatitis.3 Dermal ulcers occur in 6% of patients on panitumumab.4 Did panitumumab cause or contribute to the development of this ulcer?
Methods: The patient’s pouch system was modified to a one-piece flexible pouch system to eliminate any pressure from the flange. The hernia belt was limited to eating and activity. A hypochlorous acid topical solution was used to cleanse the ulcer. Initially, a silver hydrofiber dressing was used. The plan of care was changed to cadexomer iodine gel with a hydrofiber dressing when the ulcer continued to increase in size. A treatment break from panitumumab was initiated due to the patient’s toxicities. Her hernia surgery was then scheduled.
Results: The ulcer epithelialized 6 weeks after the panitumumab was discontinued. The hernia surgery was also performed at that time.
Discussion:
Dermatological issues can occur under an ostomy pouch system. A wound care provider must evaluate wound and ostomy patients holistically to determine all potential causes and contributing factors effecting peristomal ulcers.

.jpg)