Clinical Research
(CR-040) Analyzing the Pattern of Fracture After Pedal Level Amputation
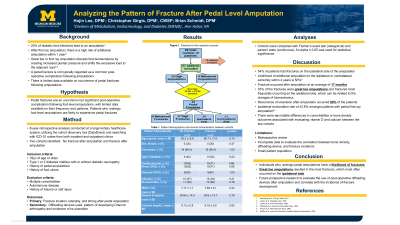
Diabetes is the leading cause of non-traumatic lower extremity amputations in the U.S., with 20% of diabetic foot infections resulting in amputation. While many studies address post-amputation complications, fracture patterns following amputation remain poorly understood. This study aims to evaluate fracture complications after pedal-level amputations in patients with diabetes.
Methods:
This 8-year retrospective study was conducted at a large tertiary health system with a single electronic medical record utilizing a cohort discovery tool (DataDirect) using ICD-9/10 codes of patients that underwent pedal level amputations with type 1 or 2 diabetes mellitus. Exclusion criteria included fractures prior to amputation or a history of bilateral lower extremity amputations. A total of 96 charts were reviewed to assess amputation and fracture location, timing, and the development of Charcot neuroarthropathy.
Results:
20 patients with 24 foot fractures met the inclusion criteria, with the average time of fracture being 16.9 months (Standard Deviation SD 12.85). 66.7% (n=16) of the fractures were ipsilateral to the side of the amputation with 1/3 (n=8) of the fractures occuring after great toe amputation. Fractures primarily occuring at adajacent digits and metatarsals. 5 cases of Charcot (25%) were identified in the post-operative period with all cases being on the ipsilateral side of the amputation with an average onset of 36.8 months.
Discussion:
Great toe amputations were most likely to result in fractures, and Charcot neuroarthropathy occurred on the ipsilateral side. These findings lay the groundwork for a prospective evaluation of this clinical query, with a focus on strategies to mitigate fracture risks.

.jpg)