Laboratory Research
(LR-021) Anti-microbial Efficacy of Silicone-based Nitric Oxide-releasing Wound Dressings in a Dermal Porcine Wound Model
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Ivan Jozic, PhD – Research Assistant Professor, Dermatology, University of Miami Miller School of Medicine; Joel Gil, BS – Sr. Manager, Research Laboratory, Dermatology, University of Miami Miller School of Medicine; Michael Solis, MBA – Sr. Research Associate 1, Dermatology, University of Miami Miller School of Medicine; Ryan Strong, BS – Research Associate, Dermatology, University of Miami Miller School of Medicine; Roger Cassagnol, BS – Research Assistant, Dermatology, University of Miami Miller School of Medicine; Beatriz Abdo Abujamra, BS – Research Associate, Dermatology, University of Miami Miller School of Medicine; Elizabeth Brisbois, PhD – Nytricx, Inc.; Hitesh Handa, PhD – Nytricx, Inc.; Ronald Shebuski, PhD – President & CEO, Nytricx, Inc.; Stephen Davis, BS – Research Professor, Dermatology, University of Miami Miller School of Medicine
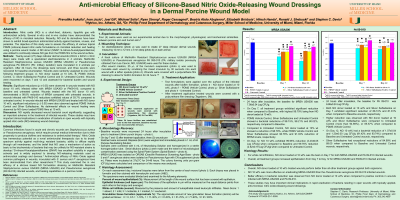
Introduction: Nitric oxide (NO) is a short-lived, diatomic, lipophilic gas with antimicrobial activity. Several in-vitro and in-vivo studies have demonstrated the efficacy of NO in microbial reduction. Recently, NO and its derivatives have been shown to exhibit broad-spectrum antimicrobial activity against bacteria, viruses, and parasites. The objective of this study was to assess the efficacy of various topical PDMS (silicone)-based nitric oxide formulations on microbial reduction and healing using a porcine wound model. A NO donor (SNAP; S-nitroso-N-acetylpenicillamine) was utilized to continually release NO gas from the PDMS film to the wound surface.
Methods: Thirty-three (33) deep reticular dermal wounds (22mm x 22mm x 3mm deep) were made with a specialized electrokeratome in 4 animals. Methicillin Resistant Staphylococcus aureus USA300 (MRSA USA300) or Pseudomonas aeruginosa PA 090-010 (PA: military isolation) were inoculated in 2 animals per organism. After 24 hours, the dressings were removed, and three wounds were recovered for baseline enumeration. Wounds were randomly assigned to one of the following treatment groups: A- NO donor loaded at 10 wt%, B- PDMS Vehicle Control, C- Silver Sulfadiazine Positive Control and D- Untreated Control. Wounds were recovered on days 7 and 12 and assessed for bacterial burden and wound healing.
Results: Significant reductions (p ≤ 0.05) were observed in wounds treated with NO donor 10 wt% infected either with MRSA USA300 or PA09-010, compared to baseline and untreated control. Wounds treated with the NO donor 10 wt% demonstrated a 99.8% reduction of MRSA compared with untreated wounds. In wounds infected with PA09-010 reductions exhibited values of 93.7% compared to untreated control. In wounds infected with MRSA USA300 and treated with NO donor 10 wt%, significant reductions (p ≤ 0.05) were also observed against PDMS Vehicle Control and Silver Sulfadiazine. No detrimental effects on wound healing were observed by NO donor loaded PDMS films at 10 wt%.
Discussion: NO rapidly decreased wound bacterial count significantly, suggesting an important advance in the treatment of infected wounds. These studies may have important clinical implications in eradication of bacteria in open wounds with topically applied nitric oxide (NO)-releasing wound dressings.
Methods: Thirty-three (33) deep reticular dermal wounds (22mm x 22mm x 3mm deep) were made with a specialized electrokeratome in 4 animals. Methicillin Resistant Staphylococcus aureus USA300 (MRSA USA300) or Pseudomonas aeruginosa PA 090-010 (PA: military isolation) were inoculated in 2 animals per organism. After 24 hours, the dressings were removed, and three wounds were recovered for baseline enumeration. Wounds were randomly assigned to one of the following treatment groups: A- NO donor loaded at 10 wt%, B- PDMS Vehicle Control, C- Silver Sulfadiazine Positive Control and D- Untreated Control. Wounds were recovered on days 7 and 12 and assessed for bacterial burden and wound healing.
Results: Significant reductions (p ≤ 0.05) were observed in wounds treated with NO donor 10 wt% infected either with MRSA USA300 or PA09-010, compared to baseline and untreated control. Wounds treated with the NO donor 10 wt% demonstrated a 99.8% reduction of MRSA compared with untreated wounds. In wounds infected with PA09-010 reductions exhibited values of 93.7% compared to untreated control. In wounds infected with MRSA USA300 and treated with NO donor 10 wt%, significant reductions (p ≤ 0.05) were also observed against PDMS Vehicle Control and Silver Sulfadiazine. No detrimental effects on wound healing were observed by NO donor loaded PDMS films at 10 wt%.
Discussion: NO rapidly decreased wound bacterial count significantly, suggesting an important advance in the treatment of infected wounds. These studies may have important clinical implications in eradication of bacteria in open wounds with topically applied nitric oxide (NO)-releasing wound dressings.

.jpg)