Case Series/Study
(CS-109) Application of Fragmented Fish Skin Graft* on Nonhealing Traumatic Leg Ulcer for an Obese Patient with Pacemaker, Metabolic Syndrome, Hypertension, and Hyperlipidemia
Venous Insufficiency
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Samera Taki, BS – Clinical Research Coordinator, Mobile Doctor Medical Clinic
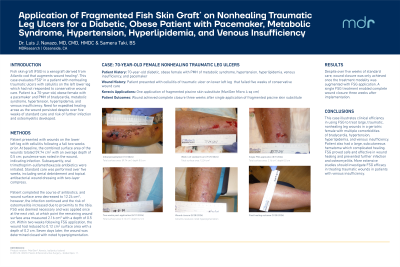
Introduction: Fish skin graft (FSG) is a xenograft derived from Atlantic cod that augments wound healing1. This case evaluates FSG* in a patient with nonhealing traumatic ulcers with cellulitis on the left lower leg which had not responded to conservative wound care. Patient is a 70-year-old, obese female with a pacemaker and PMH of bradycardia, metabolic syndrome, hypertension, hyperlipidemia, and venous insufficiency. Need for expedited healing arose as the wound persisted despite over five weeks of standard care and risk of further infection and osteomyelitis developed.
Methods: Patient presented with cellulitis on the lower left leg following a fall two weeks prior. At baseline, the combined surface area of the wounds totaled 59.74 cm2 with an average depth of 0.5 cm; purulence was noted in the wound, indicating infection. Subsequently, oral trimethoprim-sulfamethoxazole antibiotics were initiated. Standard care was performed over five weeks, including serial debridement and topical antibacterial wound dressing with two-layer compress. Patient completed the course of antibiotics, however, the infection continued and the risk of osteomyelitis increased due to proximity to the tibia. FSG was deemed necessary and was applied once at the next visit, at which point the remaining wound surface area measured 2.16 cm2 with a depth of 0.5 cm. Within two weeks following FSG application, the wound had reduced to 0.12 cm2 surface area with a depth of 0.2 cm. Seven days later, the wound was determined closed with noted hyperpigmentation.
Results: Despite over five weeks of standard care, wound closure was only achieved once the treatment modality was augmented with FSG application. A single FSG treatment enabled complete wound closure three weeks after implementation.
Discussion: This case illustrates clinical efficiency in using FSG to treat large, traumatic, nonhealing leg wounds in a geriatric female with multiple comorbidities of bradycardia, hypertension, hyperlipidemia, and venous insufficiency. Patient also had a large, subcutaneous hematoma which complicated healing. FSG proved safe and effective in wound healing and prevented further infection and osteomyelitis. More extensive studies should investigate FSG efficacy in treating traumatic wounds in patients with venous insufficiency.
Methods: Patient presented with cellulitis on the lower left leg following a fall two weeks prior. At baseline, the combined surface area of the wounds totaled 59.74 cm2 with an average depth of 0.5 cm; purulence was noted in the wound, indicating infection. Subsequently, oral trimethoprim-sulfamethoxazole antibiotics were initiated. Standard care was performed over five weeks, including serial debridement and topical antibacterial wound dressing with two-layer compress. Patient completed the course of antibiotics, however, the infection continued and the risk of osteomyelitis increased due to proximity to the tibia. FSG was deemed necessary and was applied once at the next visit, at which point the remaining wound surface area measured 2.16 cm2 with a depth of 0.5 cm. Within two weeks following FSG application, the wound had reduced to 0.12 cm2 surface area with a depth of 0.2 cm. Seven days later, the wound was determined closed with noted hyperpigmentation.
Results: Despite over five weeks of standard care, wound closure was only achieved once the treatment modality was augmented with FSG application. A single FSG treatment enabled complete wound closure three weeks after implementation.
Discussion: This case illustrates clinical efficiency in using FSG to treat large, traumatic, nonhealing leg wounds in a geriatric female with multiple comorbidities of bradycardia, hypertension, hyperlipidemia, and venous insufficiency. Patient also had a large, subcutaneous hematoma which complicated healing. FSG proved safe and effective in wound healing and prevented further infection and osteomyelitis. More extensive studies should investigate FSG efficacy in treating traumatic wounds in patients with venous insufficiency.

.jpg)