Case Series/Study
(CS-156) 1 Year Retrospective Case Series: Wound Outcomes Utilizing Novel Hydro-desloughing Wound Dressing*
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Laurel Adams, BS – MA, Plastics Division, Tulane School of Medicine; Dylan Wolff, MD – PGY-4 General Surgery Resident, Surgery, Tulane School of Medicine; Madison Vick, MS – MS3, Tulane School of Medicine; Samantha Morin, BS – MS3, Tulane School of Medicine; Abigail Chaffin, MD, FACS, CWSP, MAPWCA – Chief - Division of Plastic and Reconstructive Surgery, Surgery, Tulane School of Medicine
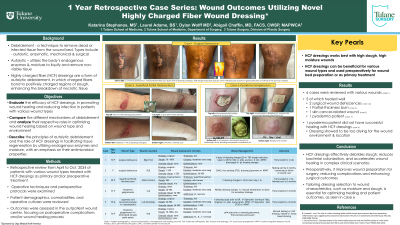
Introduction: Wound healing, a complex process, often requires debridement to remove dead or infected tissue. Debridement methods include autolytic, enzymatic, mechanical, and surgical, chosen based on wound type. Autolytic debridement, a non-invasive method, uses the body’s enzymes and moisture to liquefy non-viable tissue, promoting repair and regeneration. Hydro-desloughing dressings* enhance this process by bonding to slough and disrupting necrotic tissue. The dressing combines antimicrobial properties with autolytic benefits, offering a multifaceted approach to wound care.
Methods: Data was collected through a retrospective review of patients with various wound types, treated with hydro-desloughing dressings* as primary care or preoperative preparation to surgical management. Six qualifying patients at a single academic hospital from April-October 2024 were analyzed. Demographics, comorbidities, cultures, operative techniques, and perioperative protocols were documented. Outcomes included postoperative complications and wound healing progress.
Results: Six patients had diverse wound types: surgical wound dehiscence, pyoderma gangrenosum, partial-thickness burn, and an open wound after skin cancer excision with exposed bone and osteomyelitis. The hydro-desloughing dressing* proved especially effective for two surgical dehiscence cases, the open skin cancer-related wound, and the partial-thickness burn. Two patients with pyoderma gangrenosum showed reduced bacterial colonization on bedside fluorescence imaging. One pyoderma patient achieved full epithelialization and wound healing. The other, with a distal lower extremity wound and exposed tendon, did not. The hydro-desloughing dressing* was too drying for the wound’s location and etiology.
Discussion: This case series highlights hydro-desloughing dressings* as an effective adjunct to wound care in both clinical and perioperative settings. In the latter, it proved beneficial in treating and preparing slough-covered wounds for reconstructive surgery, supporting more efficient interventions and reducing postoperative complications. Proper dressing selection based on wound characteristics, such as slough and moisture, is crucial. Honey-based dressings may be better for minimally sloughed or dry wounds, as they promote a moist environment without excessive dryness. Conversely, wounds with significant slough benefit from absorbent dressings*, which remove devitalized tissue, reduce bacterial colonization, and manage exudate, resulting in a cleaner wound bed. Tailoring dressing selection to moisture and slough levels optimizes the wound environment, enhances healing, and patient outcomes.
Methods: Data was collected through a retrospective review of patients with various wound types, treated with hydro-desloughing dressings* as primary care or preoperative preparation to surgical management. Six qualifying patients at a single academic hospital from April-October 2024 were analyzed. Demographics, comorbidities, cultures, operative techniques, and perioperative protocols were documented. Outcomes included postoperative complications and wound healing progress.
Results: Six patients had diverse wound types: surgical wound dehiscence, pyoderma gangrenosum, partial-thickness burn, and an open wound after skin cancer excision with exposed bone and osteomyelitis. The hydro-desloughing dressing* proved especially effective for two surgical dehiscence cases, the open skin cancer-related wound, and the partial-thickness burn. Two patients with pyoderma gangrenosum showed reduced bacterial colonization on bedside fluorescence imaging. One pyoderma patient achieved full epithelialization and wound healing. The other, with a distal lower extremity wound and exposed tendon, did not. The hydro-desloughing dressing* was too drying for the wound’s location and etiology.
Discussion: This case series highlights hydro-desloughing dressings* as an effective adjunct to wound care in both clinical and perioperative settings. In the latter, it proved beneficial in treating and preparing slough-covered wounds for reconstructive surgery, supporting more efficient interventions and reducing postoperative complications. Proper dressing selection based on wound characteristics, such as slough and moisture, is crucial. Honey-based dressings may be better for minimally sloughed or dry wounds, as they promote a moist environment without excessive dryness. Conversely, wounds with significant slough benefit from absorbent dressings*, which remove devitalized tissue, reduce bacterial colonization, and manage exudate, resulting in a cleaner wound bed. Tailoring dressing selection to moisture and slough levels optimizes the wound environment, enhances healing, and patient outcomes.

.jpg)