Case Series/Study
(CS-120) Traumatic Degloving Injury: A Case Study
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Kim Abrams, DPM, PGY-2; Madison Bennett, DPM, PGY-1; Michael Broussard, DPM, PGY-2; Roxana Toth, DPM, PGY-2
Introduction:
Methods: Case Summary
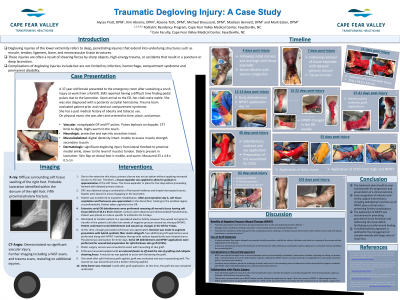
A 37-year-old female presented to the emergency department following a crush injury sustained from a forklift at work. Emergency Medical Services (EMS) reported difficulty in locating pedal pulses due to significant laceration. Upon arrival, the patient's vital signs were stable, although she was found to have a posterior occipital hematoma. The trauma team conducted an evaluation and ruled out compartment syndrome. AOx3
The patient has a past medical history notable for obesity and tobacco use.
This case study will outline the treatment course, including the utilization of negative pressure wound vacuum therapy, installation of wound vacuum therapy, synthetic grafts, split-thickness skin grafts, and application of external fixation. Collaboration with the plastic surgery team was essential in securing a sufficiently large graft to cover the wound bed, which measured 34 x 45 x 3.5 cm.
Results: NPWT: Promotes the adherence of the skin graft to the underlying tissue by creating a controlled vacuum environment with removes excess fluid and reduces hematoma or seroma formation.
Grafts: A hybrid synthetic fiber matrix allograft was selected initially to provide a scaffold for cellular infiltration and allow for cleansing of the wound without degradation of the material. A STSG was employed to enhance the formation of the skin barrier while achieving a cosmetically superior appearance, as the graft closely resembled the surrounding skin
Plastics: Plastics team recommended use of NPWT before transfer, followed by application of a graft. Given the success of NPWT in addressing the tissue deficit, patient became an appropriate candidate for a STSG, which was performed at our facility with the assistance of our own plastic surgery team.
Discussion: The treatment plan should be ever evolving with the progression and presentation of a clinical outcome.
Early recognition of infection and timely surgical interventions, including debridement and the use of NPWT, play a critical role in preventing further complications.
The application of NPWT was instrumental in promoting granulation tissue formation and addressing the tissue deficit, facilitating successful wound healing.
A multidisciplinary approach is optimal for the management of complex wounds with large areas of tissue loss.
- Degloving injuries of the lower extremity refers to deep, penetrating injuries that extend into underlying structures such as muscle, tendon, ligament, bone, and neurovascular tissue structures.
- These injuries are often a result of shearing forces by sharp objects, high-energy trauma, or accidents that result in a puncture or deep laceration.
Methods: Case Summary
A 37-year-old female presented to the emergency department following a crush injury sustained from a forklift at work. Emergency Medical Services (EMS) reported difficulty in locating pedal pulses due to significant laceration. Upon arrival, the patient's vital signs were stable, although she was found to have a posterior occipital hematoma. The trauma team conducted an evaluation and ruled out compartment syndrome. AOx3
The patient has a past medical history notable for obesity and tobacco use.
This case study will outline the treatment course, including the utilization of negative pressure wound vacuum therapy, installation of wound vacuum therapy, synthetic grafts, split-thickness skin grafts, and application of external fixation. Collaboration with the plastic surgery team was essential in securing a sufficiently large graft to cover the wound bed, which measured 34 x 45 x 3.5 cm.
Results: NPWT: Promotes the adherence of the skin graft to the underlying tissue by creating a controlled vacuum environment with removes excess fluid and reduces hematoma or seroma formation.
Grafts: A hybrid synthetic fiber matrix allograft was selected initially to provide a scaffold for cellular infiltration and allow for cleansing of the wound without degradation of the material. A STSG was employed to enhance the formation of the skin barrier while achieving a cosmetically superior appearance, as the graft closely resembled the surrounding skin
Plastics: Plastics team recommended use of NPWT before transfer, followed by application of a graft. Given the success of NPWT in addressing the tissue deficit, patient became an appropriate candidate for a STSG, which was performed at our facility with the assistance of our own plastic surgery team.
Discussion: The treatment plan should be ever evolving with the progression and presentation of a clinical outcome.
Early recognition of infection and timely surgical interventions, including debridement and the use of NPWT, play a critical role in preventing further complications.
The application of NPWT was instrumental in promoting granulation tissue formation and addressing the tissue deficit, facilitating successful wound healing.
A multidisciplinary approach is optimal for the management of complex wounds with large areas of tissue loss.

.jpg)