Case Series/Study
(CS-161) Scleroderma Skin Ulcers: Ovine Extracellular Matrix with Hyaluronic Acid Xenograft, a Promising Approach to an Orphan Disease
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Michelle Moore, RN – Kaleidoscope Clinical Consulting; Katrina-Anne Palu, Podiatrist – Vaiola Hospital; Nya Akoteu, RN – Vaiola Hospital
Introduction:
Systemic sclerosis (SSc), commonly referred to as scleroderma, is a chronic autoimmune rheumatic disease affecting multiple systems. Excessive fibrosis, blood vessel abnormalities, and immune system disruptions mark this rare condition. When SSc impacts only the skin, it is categorized as "localized" scleroderma. The aim was to observe the response of a hard-to-heal scleroderma skin ulcer on the right fourth finger of a 54-year-old diabetic female after initiating the routine application of a xenograft composed of a layer of glycosaminoglycans (hyaluronic acid) between sheets of ovine forestomach-derived extracellular matrix (ECM).
Methods:
The setting of this case report was a hospital-based outpatient diabetic wound care clinic at Vaiola Hospital, Nuku’alofa, the main hospital in the Kingdom of Tonga. In Tonga, there is limited availability of chemotherapy or immunotherapy for treating systemic sclerosis. After remaining refractory for three months to standard wound care, a cellular, acellular, matrix-like product (CAMP) was added to the patient’s wound care treatment regimen. The standard of care techniques was continued while incorporating a xenograft composed of a layer of glycosaminoglycans (hyaluronic acid) between sheets of ovine forestomach-derived extracellular matrix (ECM) (Symphony*, Aroa Biosurgery, Auckland, New Zealand).
Results:
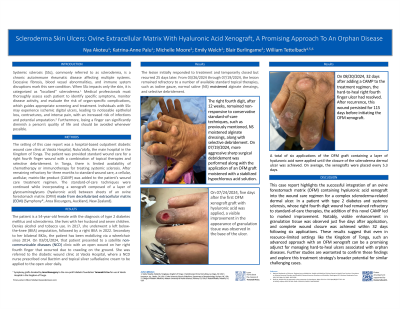
The patient was a 54-year-old female with the diagnosis of type 2 diabetes mellitus and scleroderma. She underwent a left below-the-knee (BKA) amputation, followed by a right BKA in 2022. A1C was 11%. She has been mobilizing via a wheelchair since 2014. On 03/01/2024, that patient presented to a satellite non-communicable diseases clinic with an open wound on her right fourth finger that occurred due to crawling on the ground. From 03/26/2024 through 07/19/2024, the lesion remained refractory to a number of available standard topical therapies, such as iodine gauze, moistened alginate dressings and selective debridement. A total of six applications of the ovine ECM graft containing a layer of hyaluronic acid were applied until the closure of the scleroderma skin ulcer was achieved. On average, the xenografts were placed every 5.3 days.
Discussion:
Routine applications of an ovine ECM with hyaluronic acid were observed to reinitiate the trajectory towards closure with reductions in wound size and observed an increase in granulation tissue despite the underlying commodities of poorly controlled diabetes and systemic sclerosis. The results suggest a potential novel treatment option for hard-to-heal wounds in patients with scleroderma. Ovine ECM xenografts with hyaluronic acid treatment should be formally evaluated as an adjunct treatment for refractory scleroderma ulcers.
Systemic sclerosis (SSc), commonly referred to as scleroderma, is a chronic autoimmune rheumatic disease affecting multiple systems. Excessive fibrosis, blood vessel abnormalities, and immune system disruptions mark this rare condition. When SSc impacts only the skin, it is categorized as "localized" scleroderma. The aim was to observe the response of a hard-to-heal scleroderma skin ulcer on the right fourth finger of a 54-year-old diabetic female after initiating the routine application of a xenograft composed of a layer of glycosaminoglycans (hyaluronic acid) between sheets of ovine forestomach-derived extracellular matrix (ECM).
Methods:
The setting of this case report was a hospital-based outpatient diabetic wound care clinic at Vaiola Hospital, Nuku’alofa, the main hospital in the Kingdom of Tonga. In Tonga, there is limited availability of chemotherapy or immunotherapy for treating systemic sclerosis. After remaining refractory for three months to standard wound care, a cellular, acellular, matrix-like product (CAMP) was added to the patient’s wound care treatment regimen. The standard of care techniques was continued while incorporating a xenograft composed of a layer of glycosaminoglycans (hyaluronic acid) between sheets of ovine forestomach-derived extracellular matrix (ECM) (Symphony*, Aroa Biosurgery, Auckland, New Zealand).
Results:
The patient was a 54-year-old female with the diagnosis of type 2 diabetes mellitus and scleroderma. She underwent a left below-the-knee (BKA) amputation, followed by a right BKA in 2022. A1C was 11%. She has been mobilizing via a wheelchair since 2014. On 03/01/2024, that patient presented to a satellite non-communicable diseases clinic with an open wound on her right fourth finger that occurred due to crawling on the ground. From 03/26/2024 through 07/19/2024, the lesion remained refractory to a number of available standard topical therapies, such as iodine gauze, moistened alginate dressings and selective debridement. A total of six applications of the ovine ECM graft containing a layer of hyaluronic acid were applied until the closure of the scleroderma skin ulcer was achieved. On average, the xenografts were placed every 5.3 days.
Discussion:
Routine applications of an ovine ECM with hyaluronic acid were observed to reinitiate the trajectory towards closure with reductions in wound size and observed an increase in granulation tissue despite the underlying commodities of poorly controlled diabetes and systemic sclerosis. The results suggest a potential novel treatment option for hard-to-heal wounds in patients with scleroderma. Ovine ECM xenografts with hyaluronic acid treatment should be formally evaluated as an adjunct treatment for refractory scleroderma ulcers.

.jpg)