Practice Innovations
(PI-049 (RPT-010)) From Pressure to Prevention: Elevating Care in the Intensive Care Unit
Friday, May 2, 2025
4:45 PM - 5:45 PM East Coast USA Time
Introduction: Sacral gluteal Hospital Acquired Pressure Injuries (HAPIs), a form of skin breakdown, commonly affect ICU patients due to decreased mobility and poor hemodynamics. HAPIs have long term effects on patients’ skin integrity, quality of life, and increase hospital costs. Literature shows turning reduces the incidence of HAPIs. Audits validate low turning compliance. Compared with traditional repositioning devices, Air Assisted Repositioning Devices (AARD's) are more accessible for frequent patient repositioning, effectively offload the sacrum, and decrease strain to staff.
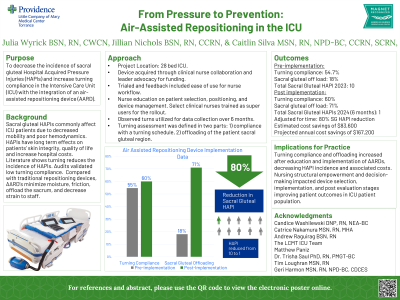
Methods: This quality improvement project was implemented on a 28 bed ICU. AARD's were acquired through clinical nurse collaboration and leader advocacy for funding. The device was trialed and feedback included ease of use for nurse workflow, including ability to keep device under patient for frequent use. Nurses received education on patient selection, positioning, and device management. Select clinical nurses were trained as super users. Pre implementation data consisted of 90 observed turn assessments. Post implementation data was collected over 6 months. Turning assessment compliance was defined as: 1) adherence to the turning schedule, 2) offloading of the patient sacral gluteal region.
Results: Implementation occurred in April 2024. 2024 ICU pre implementation turning compliance, adherence to the turning schedule, was 54.7%; 18% of patients had sacral gluteal region offload. Post implementation turning compliance was 60%; 71% of patients had sacral gluteal region offload. In 2023 the ICU had 10 sacral gluteal HAPIs, six months post implementation ICU incidence decreased to one. Adjusted for time, this is an 80% reduction in sacral gluteal HAPIs in the ICU. Post implementation HAPI data outperforms national mean. Estimated cost savings of $83,600. Projected annual cost savings of $167,200. Post implementation data was disseminated during unit staff meetings.
Discussion: Turning compliance and offloading increased after education and implementation of AARDs, decreasing HAPI incidence and associated costs in the ICU. Nursing structural empowerment and decision-making impacted device selection, implementation, and post evaluation stages improving patient outcomes.
Methods: This quality improvement project was implemented on a 28 bed ICU. AARD's were acquired through clinical nurse collaboration and leader advocacy for funding. The device was trialed and feedback included ease of use for nurse workflow, including ability to keep device under patient for frequent use. Nurses received education on patient selection, positioning, and device management. Select clinical nurses were trained as super users. Pre implementation data consisted of 90 observed turn assessments. Post implementation data was collected over 6 months. Turning assessment compliance was defined as: 1) adherence to the turning schedule, 2) offloading of the patient sacral gluteal region.
Results: Implementation occurred in April 2024. 2024 ICU pre implementation turning compliance, adherence to the turning schedule, was 54.7%; 18% of patients had sacral gluteal region offload. Post implementation turning compliance was 60%; 71% of patients had sacral gluteal region offload. In 2023 the ICU had 10 sacral gluteal HAPIs, six months post implementation ICU incidence decreased to one. Adjusted for time, this is an 80% reduction in sacral gluteal HAPIs in the ICU. Post implementation HAPI data outperforms national mean. Estimated cost savings of $83,600. Projected annual cost savings of $167,200. Post implementation data was disseminated during unit staff meetings.
Discussion: Turning compliance and offloading increased after education and implementation of AARDs, decreasing HAPI incidence and associated costs in the ICU. Nursing structural empowerment and decision-making impacted device selection, implementation, and post evaluation stages improving patient outcomes.

.jpg)
